|
||||||||||||||||||||||||||
| March 7, 2024 | ||||||||||||||||||||||||||
Safety is the highest priority for both consumers and providers of care in the community.
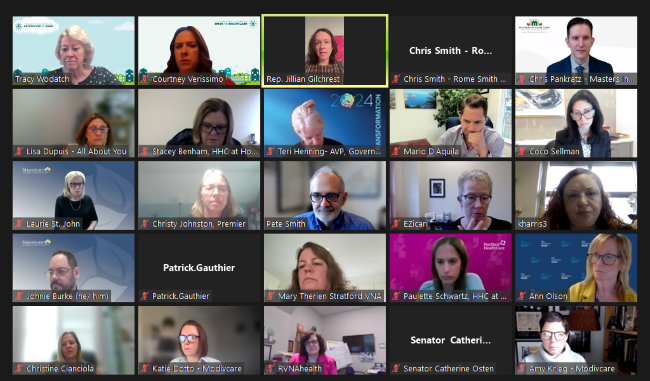
Yesterday, the Connecticut Association for Healthcare at Home hosted its virtual Annual Legislative Advocacy Day. Nearly 35 members and a dozen legislators joined the meeting. The Association’s 2024 legislative priorities based on recent legislative bills and hearings were discussed, and the meeting also provided an opportunity for legislators and members to ask questions and offer opinions.
Safety and workplace violence prevention are top priorities along with funding to support any mandated trainings or need for additional staff/technology. Several bills are targeting these areas, giving home care avenues to add recommendations, support and collaboration to enhance protections for both providers and consumers of care.
Members are strongly encouraged to reach out to their legislators based on both their home address and their office address using this list of 2024 legislators with phone and email address included.
Several bills pertaining to home and community-based services were heard before the Aging Committee on Tuesday, March 5, including HB 5001 An Act Supporting CT Seniors and the Improvement of Nursing and Home-Based Care.
Association Pres/CEO Tracy Wodatch testified in partial support along with citing challenges within certain proposals.
Highlights within the bill include:
Additional bills heard regarding home and community-based services were:
Below are links to the written testimony as submitted by the Association and its members:
Source: CDC, March 1, 2024
On March 1, CDC released updated recommendations for how people can protect themselves and their communities from respiratory viruses, including COVID-19. The new guidance brings a unified approach to addressing risks from a range of common respiratory viral illnesses, such as COVID-19, flu, and RSV, which can cause significant health impacts and strain on hospitals and health care workers. CDC is making updates to the recommendations now because the U.S. is seeing far fewer hospitalizations and deaths associated with COVID-19 and because we have more tools than ever to combat flu, COVID, and RSV.
Source: CT DPH
HARTFORD, Conn—The Connecticut Department of Public Health (DPH) has adopted and recommends the COVID-19 isolation guidance that was issued by the Centers for Disease Control and Prevention (CDC) on Friday.
This updated guidance recommends that those who have COVID-19 should stay home until they’ve been fever-free without medication for at least 24 hours or their symptoms have been improving for 24 hours.
Since the start of the 2023—2024 respiratory virus season, DPH has taken a pan-respiratory virus approach to managing COVID-19, the flu and RSV. This strategy has been consistent with the CDC guidance for managing viral respiratory diseases including COVID-19, influenza, and RSV.
Additionally, prior to the start of the current school year, DPH partnered with the Connecticut State Department of Education to distribute operationalized CDC respiratory virus guidance to school nurses and superintendents.
Source: NAHC, Feb. 29, 2024
On Monday, Feb. 26, NAHC President Bill Dombi, Senior Director of Government Affairs Calvin McDaniel, and Director of Medicaid Advocacy Damon Terzaghi were joined by NAHC Board Members David Totaro and Jennifer Sheets in a meeting with the Office of Management and Budget at the White House.
In the meeting, which was also attended by several staff from the Centers for Medicare and Medicaid Services, the NAHC representatives outlined the potential impact of the Medicaid Access rule. The representatives highlighted the negative impact on private businesses as well as the impact on state and Federal Medicaid expenditures. Specifically, NAHC raised concerns about whether the rulemaking had appropriately followed the Congressional Review Act and Administrative Procedures Act.
The Medicaid Access rule remains under review at OMB with an expected final release before the end of April.
Stay tuned for updates on the Medicaid Access Rule in NAHC Report and Medicaid Monthly. If you have any specific questions about the Medicaid Access Rule or anything to do with Medicaid, please contact Damon Terzaghi at dterzaghi@nahc.org.
Source: NHPCO, March 4, 2024
On March 4, 2024, the Centers for Medicare & Medicaid Services (CMS) announced the termination of the hospice component of the VBID Model, effective December 31, 2024. CMS cited feedback from providers, beneficiaries, and MA Organizations (MAOs) about their experience with VBID as the reason for discontinuing the hospice component of the model. CMS will no longer be accepting applications for the calendar year (CY) 2025 Request for Applications. This means hospice will no longer be a part of the VBID model beginning January 1, 2025. Hospice providers currently contracted with MAOs will continue with their contracts for CY 2024. CMS will issue additional guidance later this year.
Source: NAHC, Feb. 28, 2024
Hospice Provider Enrollment Changes
The Centers for Medicare & Medicaid Services (CMS) officials reviewed hospice provider enrollment requirements that revised the definition of managing employee to include hospice administrator and hospice Medical Director. The announcement generated several questions from hospice providers. CMS officials clarified that an individual that manages the day-to-day operations of the facility is considered a managing employee which could include supervisors within the hospice. Because a Medical Director designee would only be in place if the normal Medical Director was unavailable, they wouldn’t need to report a designee as a managing employee. Contracted staff are to be reported as managing employees. Hospices are to report on Form 855-A for initial enrollment and on a change of ownership (CHOW) or change in majority ownership (CIMO) form if there is a change in ownership. Any further questions can be submitted to ProviderEnrollment@cms.hhs.gov.
Source: NAHC, March 4, 2024
One of the top medical review denial reasons for hospices is an invalid Medicare election statement. This statement is required for each Medicare beneficiary receiving hospice services. If the statement does not contain all the required elements it could result in claim denials.
In the fiscal year (FY) 2020 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Requirements final rule, the Centers for Medicare & Medicaid Services (CMS) finalized modifications to the hospice election statement content requirements at §418.24(b) and added a hospice election statement addendum requirement at §418.24(c). CMS then made clarifying modifications in the FY 2022 Hospice Wage Index and Payment Rate Update, Hospice Conditions of Participation Updates, Hospice and Home Health Quality Reporting Program Requirements final rule. The modifications and additions to the election statement increase coverage transparency for beneficiaries electing hospice care.
Source: Corcoran Consulting Group, March 6, 2024
Corcoran Consulting Group LLC is pleased to welcome healthcare leader Nancy Scheetz, APRN, as Managing Consultant. Nancy works closely with Corcoran team members to actively support the operational, clinical, and financial goals of its home care agency clients.
Scheetz brings over 40 years of professional experience in health care, focusing on behavioral health, addiction services, home health care, and hospice.
Before joining Corcoran Consulting Group, she was CEO of a Connecticut-based non-profit, licensed home care and hospice organization. In that role, she improved quality and increased revenue through innovation initiatives, quality assurance, clinical standards, fiscal management, contract expansion, and board development. The measures Scheetz implemented dramatically increased home health and hospice patient referrals and patient census, aligned the organization with value-based purchasing, and paved the way for a successful merger.
|
||||||||||||||||||||||||||
| Past Issues | Subscribe | cthealthcareathome.org | Advertise with Us | ||||||||||||||||||||||||||