|
||||||||||||||||||||||
| April 11, 2024 | ||||||||||||||||||||||
Source: Hartford Courant
In a rare move, a key legislative committee has refused to vote as lawmakers are leaving the state budget largely intact as they head toward final negotiations with Gov. Ned Lamont in the coming month.
The legislature traditionally makes a series of changes — large and small — in the package that the governor unveils in early February. But this year, lawmakers will instead focus on a more narrow list of top Democratic policy priorities that include public higher education, nonprofit organizations that provide state services, and mental health care for children by boosting Medicaid rates for doctors and other providers. The fiscal baseline will be the recommendations that the legislature had already approved for the second year of the two-year budget.
Source: McKnight's, March 29, 2024
The Centers for Medicare & Medicaid Services on Thursday proposed a 2.6% hospice payment update for fiscal year 2025. Providers quickly reacted unfavorably to the update.
“The 2.6% proposed rate increase for hospices is not enough to support the continued delivery of hospice care amidst rising cost pressures and ongoing workforce constraints affecting hospices nationwide,” National Hospice and Palliative Care COO and Interim CEO Ben Marcantonio said in a statement. “To continue providing the high level of care our patients and their families deserve, hospices require a payment rate that accurately reflects the current economic challenges. We know that hospice care has demonstrated $3.5 billion in annual savings for Medicare, which underscores the critical importance of investing in hospice to ensure continued beneficiary access to quality end-of-life care.”
Source: NAHC, April 5, 2024
For this refresh, Home Health (HH) Outcome and Assessment Information Set (OASIS) measures have been updated.
For additional information, please see the HH Quality Reporting Training webpage and the Home Health Data Submission Deadlines webpage.
Source: Decision Health, April 5, 2024
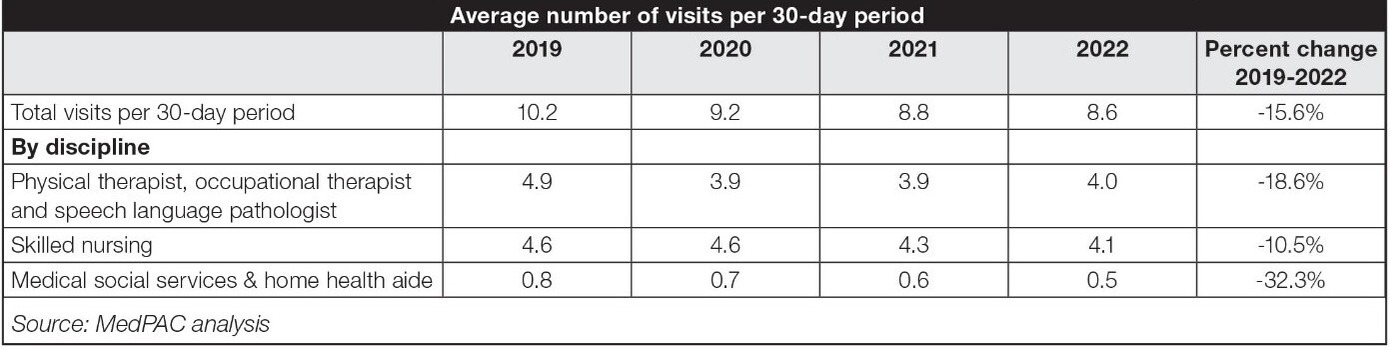
Home health aide visits have declined more than 32% over the first three years of PDGM. That’s more than twice the change in the total number of visits in a 30-day period. Source: NAHC, April 3, 2024
On Tuesday, March 12, the Centers for Medicare & Medicaid Services (CMS) released a report to Congress on Best Practices within the Medicaid Money Follows the Person deinstitutionalization program. This report was required by the Consolidated Appropriations Act of 2021, which identified eight key areas for CMS to report on best practices.
Source: McKnight's, April 2, 2024
Though the number of registered nurses continues to grow, fewer are working in home healthcare and hospice compared to years past, according to the latest national sample survey collected by the Health Resources & Services Administration.
In 2018, there were 179,509 RNs working in home health and hospice, representing about 6% of the nursing workforce, according to an earlier national survey. HRSA’s latest count estimated that there were 173,808 RNs in home health and hospice in 2022, or only 5% of the workforce. The survey was a joint effort between HRSA’s National Center for Health Workforce Analysis and the Census Bureau, and included input from more than 50,000 RNs.
Viventium, one of our associate members, just released their 2024 Caregiver Onboarding Experience Report: A Re-Think is Overdue.
Viventium surveyed 175 post-acute care administrators and 220 caregivers to gather real-life experiences during their onboarding process in an effort to dive deeper into why so many organizations are struggling to retain staff. This report provides readers with key takeaways about the onboarding, training, and payroll standards in home care and home health industries today.
Here are a few of the main drivers that led to their research:
Download their report to get the insights for re-thinking the nuts and bolts of your onboarding to better engage, motivate, and retain your top caregivers.
About Viventium — Viventium is a payroll and HR software company specializing in home-based and facility/community-based care, paying over 424,000 health services employees. With over 30 years of experience, Viventium’s flexible human capital management software suite makes it easier for clients to employ their greatest asset: their employees. To learn more about the report, schedule a meeting here with Viventium.
|
||||||||||||||||||||||
| Past Issues | Subscribe | cthealthcareathome.org | Advertise with Us | ||||||||||||||||||||||