|
|||||||||||||||||||||||||||||
| September 19, 2024 | |||||||||||||||||||||||||||||
Source: The Alliance, September 17, 2024
Hospices will begin completing the Hospice Outcome & Patient Evaluation (HOPE) on October 1, 2025. The final HOPE item sets – HOPE Admission v1.00, HOPE Update Visit (HUV) v1.00, HOPE Discharge v1.00 and HOPE ALL Item v1.00 – and accompanying HOPE Guidance Manual v1.00 were released on September 16, 2024. These documents can be accessed from the Downloads section on the CMS HQRP HOPE webpage.
The HOPE data collection tool replaces the Hospice Item Set (HIS) but includes many of the same items. CMS has provided a table outlining the changes from the HIS to the HOPE. Hospices will stop completing the HIS when HOPE is implemented next year. CMS indicated in a recent Hospice Quality Reporting Program (HQRP) Forum that there will likely be some overlap when HOPE begins and HIS ends. Presumably there will be HIS-Discharge records completed and submitted for those patients who are admitted prior to HOPE implementation but are discharged after this date. More information will be coming from CMS as the implementation date is closer. The HQRP Forum slides and transcript can be accessed in the Downloads section of the Provider and Stakeholder Engagement webpage.
Source: The Alliance
Over the summer of 2024, legacy NAHC (now the Alliance) surveyed members regarding important measures of access to Medicaid-funded home and community-based services. The survey focused on two main issues:
The survey also collected information regarding reasons why referrals are rejected and hours are left unfilled.
Important findings from the survey include:
The Alliance intends to continuously update this report to reflect additional information as it is received. If your organization has not yet responded to the survey, we encourage you to fill it out HERE.
Source: nbcnonnecticut.com
The Centers for Medicare & Medicaid Services terminated Abbott Terrace Health Center's participation in the Medicare and Medicaid programs effective September 10. While the facility, which houses 180 residents and employs 287 staff, is exploring its options in light of the decision, it also is preparing for the possibility of closure, including "identifying other locations for our residents and supporting our staff as they prepare to transfer to other Athena sites and employment opportunities in the local area."
Source: The Alliance, September 18, 2024
The Centers for Medicare & Medicaid Services (CMS) held a Home Health, Hospice & DME Open Door Forum on September 17, 2024. Below is a summary of the Forum for those unable to attend.
HOME HEALTH
The first Annual Performance Report (APR) for the Home Health Value Based Purchasing (HHVBP) program was posted in August. This preview report includes each HHA’s annual total performance score for the calendar year 2023 performance year and the associated payment adjustment that will be applied to all Medicare fee-for-service claims submitted for Home Health services through 2025.
This information will be publicly reported starting in January 2025. The recalculation request period for the preview report ended September 7, 2024. The preliminary APRs will be posted on or around September 27 once all recalculation requests are processed. The next phase of the appeals process is for reconsideration and is only available to those HHAs that submitted a recalculation request. Earlier this week, CMS made a web-based training available: Expanded HHVBP Model Web-Based Training: Changes to the Applicable Measure Set Beginning in CY 2025.
The October 2024 Care Compare preview reports will have three measures:
These will be reported for the first time on Care Compare in January 2025.
CMS updated two resources recently:
1) From Data Elements to Quality Measures Cross-Setting Web-Based Training – provides a high-level overview of how data elements are used to construct quality measures used across post-acute care settings.
2) Section GG Web-Based Training Series
HOSPICE
Care Compare hospice data will be refreshed in November 2024. The Provider Preview Reports for this refresh were released in August.
On Wednesday, August 21, 2024, the Centers for Medicare & Medicaid Services (CMS) hosted the August 2024 HQRP Forum to provide information on the Fiscal Year 2025 Hospice Final Rule and additional HQRP updates. Materials from this HQRP Forum, including a recording of the presentation, are now available in the Downloads section of the Provider and Stakeholder Engagement page. A recording of the presentation is also available on the official CMS YouTube channel: https://youtu.be/eZcIlptDelA
The HQRP Quarterly Q&A for Q2, 2024 is now available. This Q&A includes selected questions received by the Hospice Quality Help Desk during the second quarter of 2024 (Apr. 1 to June 30).
The final HOPE item sets, Guidance Manual and Change Table were recently posted to the HOPE webpage. (Please see the Alliance’s summary here.) CMS recently posted a brief explainer video, Hospice Outcomes and Patient Evaluations (HOPE) Data Collection Timepoints, and will be publishing a new web-based training that is titled Introducing the Hospice Outcomes and Patient
Evaluation – HOPE tool in the coming weeks. The HOPE data specifications will be available in October 2024. Additional information related to the transition from HIS to HOPE and information on HART submission sunsetting as well as the transition from QIES to iQIES for hospices will be provided in the coming months.
Source: FDA
The FDA has approved and authorized for emergency use updated COVID-19 vaccines (2024-2025 formula) to provide better protection against COVID-19 caused by circulating variants.
Specifically, FDA has authorized the following for emergency use:
The following COVID-19 vaccines are approved by FDA:
Source: The Alliance, September 10, 2024
The Centers for Medicare & Medicaid Services (CMS) has scheduled an upcoming training series on the home- and community-based services (HCBS) provisions of the Medicaid Access Rule. The Ensuring Access to Medicaid Services final rule (Access rule) advances access to care and quality of care, and will improve health outcomes for Medicaid beneficiaries across fee-for-service (FFS) and managed care delivery systems, including HCBS provided through those delivery systems. Specifically, the HCBS provisions of the rule make sweeping changes intended to strengthen necessary safeguards to ensure health and welfare, promote health equity for people receiving Medicaid-covered HCBS, and achieve a more consistent and coordinated approach to the administration of policies and procedures across Medicaid HCBS programs.
CMS will be hosting training sessions on several key provisions of the Access rule to ensure that all partners fully understand the various HCBS provisions within the rule as well as have an opportunity to ask questions and provide feedback on implementation of the rule. Information regarding dates of the training sessions, tentative topics for each session, and registration information can be found below.
Dates and Tentative Topics:
Where: Zoom link will be provided following registration. When you register, select all the training dates you would like to attend from the checklist. You can register for one or multiple training dates.
Who Should Attend: These trainings are open to states, state associations, advocates, health care and HCBS providers, and other partners who work with Medicaid or HCBS.
*Nursing Facility and Intermediate Care Facilities for Individuals with Intellectual Disabilities Rate Transparency provisions finalized in CMS-3442-F: Medicare and Medicaid Programs; Minimum Staffing Standards for Long-Term Care Facilities and Medicaid Institutional Payment Transparency Reporting
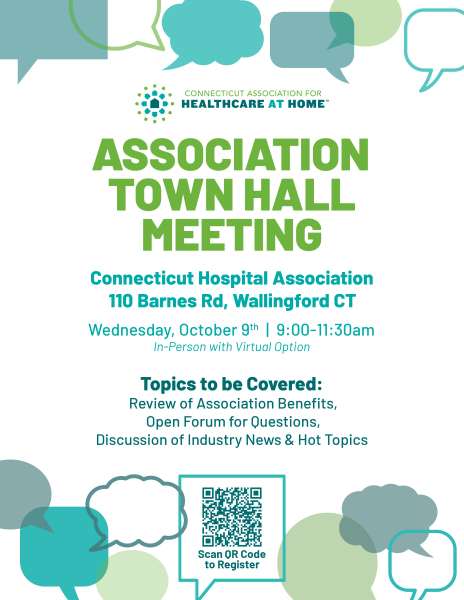
Do you want to stay updated on the latest industry trends, best practices, and innovations? Then don’t miss our Annual Conference!
This year’s conference is set to be our most impactful yet, bringing together leaders and experts from across the industry. This conference offers invaluable insights and opportunities to enhance the skills and knowledge of your entire team.
Since 1984, the founders of Preferred Care at Home have had the privilege of assisting clients improve their quality of life while still recognizing and maintaining their dignity and independence. Preferred Care at Home has continued this tradition by referring only the most reliable, compassionate, experienced, and affordable caregivers to clients' homes or care facilities.
They understand that long-term care can be costly, which is why they have focused on building a reputation of offering access to quality services at affordable prices.
Ask about the wide range of non-medical services available from 1 to 24 hours per day, and about qualified live-in caregivers who can provide 24-hour peace of mind for you or your loved one.
Providing home care services in Easton, Darien, New Canaan, Fairfield, Ridgefield, Weston, Redding, Wilton and surrounding areas.
|
|||||||||||||||||||||||||||||
| Past Issues | Subscribe | cthealthcareathome.org | Advertise with Us | |||||||||||||||||||||||||||||