BEST PRACTICES FOR DEFINING AND PRIORITIZING DEI STRATEGY AND COMMUNICATIONS
Best Practices for Defining and Prioritizing DEI Strategy and Communications
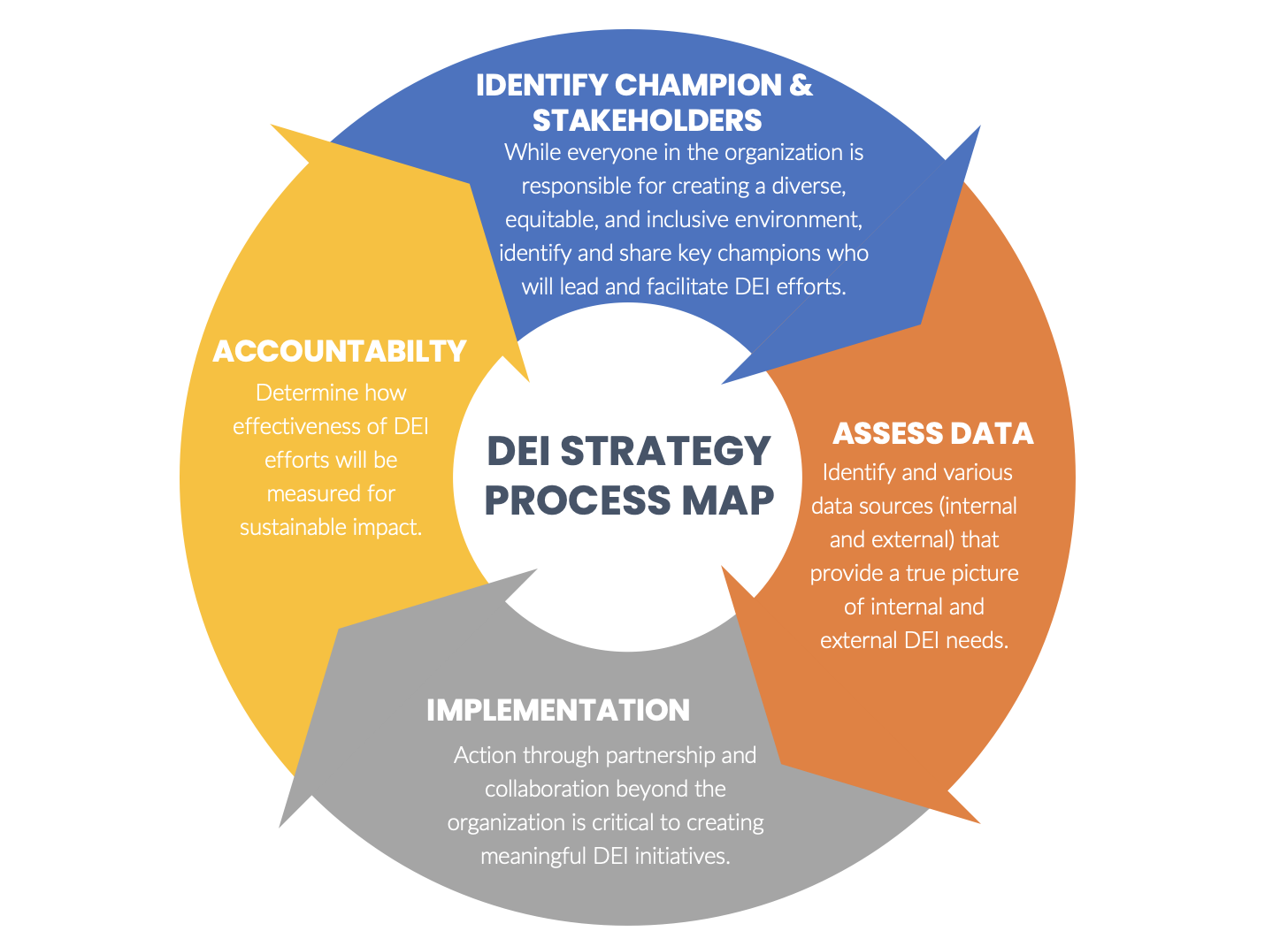
When pursuing diversity, equity and inclusion (DEI) strategy and communications at your healthcare institution, it can be tempting to dive directly into concepts for programs and interventions. However, to translate a commitment to DEI into meaningful changes in the health of the communities your institution serves, it is essential to start with the basics. These include collecting data on community needs and identifying champions for this work, according to Camille Strickland, the senior vice president of BVK, a marketing firm that incorporates a health strategy practice, in Milwaukee.
“This is very foundational work,” says Strickland, who led the conversation at a recent SHSMD Member Meet-Up on “Defining and Prioritizing DEI Strategy and Communications.” She notes that “organizations need to leverage multiple data sources to uncover both your own internal needs and your community’s needs regarding DEI, and that data comes in many different forms.”
Internal data sources may include:
- Patient demographics from electronic health records,
- Health Services/Technology Assessment Texts (or HSTAT) from the Agency for Healthcare Research and Quality,
- Prospective surveys sent to patients,
- Cultural competency surveys, and
- Human resources data on the makeup of your organization and the diversity of its workforce.
“These data points come together to tell a story of what’s happening internally in your organization and where the needs and strengths are in terms of DEI,” Strickland says.
External data sources about the community you serve can include:
- Information from your institution’s community benefits team,
- Demographic data from city and state sources,
- Information from partner organizations, and
- Data on social determinants of health from the Centers for Medicare & Medicaid Services and any government agencies at the local and state levels.
“The data you gather will be a combination of both qualitative and quantitative, and understanding the story it is telling can be very complex,” Strickland notes. “To analyze it and allow you to develop DEI strategies based on accurate conclusions, you need to identify collaborators. Area colleges and universities can often be a rich starting point; they typically have a diverse array of data analysts, statisticians and others. People in our meet-up also mentioned that nursing programs can frequently be good partners, as can grassroots community organizations with people on the ground who understand their communities.”
As an example, she cited the ANCHOR (Anal Cancer HSIL Outcomes Research) study, a large phase 3 study that released findings in 2021, showing that treating precursor anal cancer lesions can significantly reduce the risk for progression to frank anal cancer in people living with HIV. The ANCHOR investigators partnered with national and local community advisory boards that gave them insight into the concerns of all involved communities affected by the study, provided feedback on ethical and practical concerns and identified obstacles to study recruitment, and raised awareness about the study in their communities.
“This is a great example of a collaboration between a university health system, a care provider and community partners,” Strickland says. “This is the kind of approach that can help focus on problems affecting specific populations, particularly those who fall into the category of often not receiving equitable care.”
Partnerships like these are essential, agrees Cristal Herrera Woodley, the director of marketing, communications and customer engagement at Renown Regional Medical Center, in Reno, Nevada, as the first and only hospital in the state designated with a perfect score and at the highest level of support as an “LGBTQ+ Healthcare Equality Leader,” on the national Healthcare Equality Index (HEI) from the Human Rights Campaign Fund.
HEI benchmarks focus on four key areas: non-discrimination and staff training, patient services and support, employee benefits and policies, patient and community engagement, and responsible citizenship.
“Their detailed guidance and benchmarks really helped us understand where to focus our attention,” Woodley says.
In June 2021, Renown affiliated with the University of Nevada-Reno School of Medicine, becoming Nevada’s first integrated health system with missions in education, patient care and clinical research.
“They have a very robust DEI team, and that partnership allows us to expand our efforts in terms of research opportunities and engaging with medical students in our facilities,” Woodley explains. For example, Renown now works with the medical school to support “Black Men in White Coats,” a national program that seeks to increase the number of black men in the field of medicine by exposure, inspiration and mentoring.
A second DEI core imperative discussed at the SHSMD member meet-up is identifying and communicating with champions for these efforts.
“There are several different approaches across organizations,” Strickland notes. “Sometimes the champions come from the top down, via a chief equity officer or chief diversity officer or having that be a shared responsibility across several leaders. In other institutions, the leaders might set the agenda, but they’re not the in-front champions; they rely on the departments and DEI is more of a collective approach. A less common but growing model is the bottom-up approach, in which audiences like caregiver affinity groups or departmental champions with a passion for taking action drive the DEI efforts, telling leadership where they need to focus efforts based on what patients are saying about their experiences both inside and outside the hospital.”
Whoever the champions may be, DEI strategy in healthcare should strive to address barriers to good health beyond the hospital, according to Strickland.
“We talk a lot in healthcare about social determinants of health, but things like housing, transportation, health literacy and societal stigmas are enormous challenges,” she says. “You need to get outside our four walls and identify partners who are beginning to address those problems. You might not have the budget to partner with a transportation tech company to support patient transit, but could you offer shuttle services in a five-mile radius, for example? You need to understand how all these factors might be impediments to the health of people you are trying to serve, and how you might be a solution provider in that.”


