STRATEGIC PLANNING
Strategies to Move Hospital and Health Care Systems Forward in a Post-Pandemic World
There is no doubt that the COVID-19 pandemic dramatically reshaped society and the health care delivery system. More than three years after the start of the global health emergency, health care leaders continue to address some of the biggest challenges facing the industry with the rapid adoption of new strategies to drive recovery in a rapidly evolving landscape.
Operating in a new normal, hospital and health care organizations are redefining systems, changing strategic priorities, and modifying processes to answer the changing needs of communities. From workforce burnout and staffing shortages to surge capacity challenges and health equity issues, today’s leaders must learn from the past few years to effectively and successfully forge ahead, according to author, consultant and futurist Ian Morrison, PhD.
"Throughout the COVID pandemic, hospitals and health systems played a pivotal leadership role in serving their communities,” Dr. Morrison says in Futurescan—Healthcare Trends and Implications 2023.
Speaking of strategies for "a future that no one could have imagined,” he urged health care leaders to concentrate on eight key areas of strategic focus, stating that, "these new realities have become permanent fixtures in the health care environment.”
The New Realities
There is a clear roadmap for the challenges and opportunities at hand for all health care strategists. To ensure that hospital and system leaders accurately track the pulse of the industry, several key trends must be considered to move forward in the post-pandemic world. These trends are outlined below...
Workforce and staffing trends
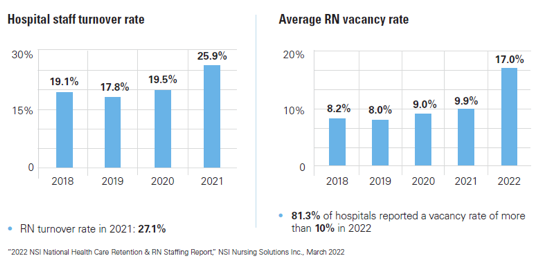
At the peak of the pandemic, frontline workers experienced life-altering stressors, leading to some of the highest levels of workforce burnout in a decade. What resulted was the "Great Resignation,” as staff who bore the heavy physical and emotional burden of the public health crisis left the field. According to Environmental Scan 2023, hospital staff turnover increased from 19% in 2018 to close to 26% by 2021, with registered nurse (RN) turnover rates exceeding 27% by 2021. Similarly, the RN vacancy rate in hospitals increased almost tenfold from 2018 when the vacancy rate was 8.2% compared to 17% by 2022.
On the physician side, burnout rates among all physicians rose from 42% in 2021 to 47% in 2022 with emergency medicine physicians experiencing the highest jump. In addition, 60% of emergency room physicians cited burnout in 2022 compared with 43% in 2021.
Identifying practices to mitigate further turnover, increase staff retention, and ramp up recruitment efforts should be a key priority for leaders in 2023. As explained in the Futurescan 2023 report, health care executives should leverage technology to improve staff efficiency, ensure that initiatives for employee retention and recruitment are sustainable, and invest in a corporate culture that connects staff to the mission of providing excellent patient care.
Consumerism and the patient experience
Shifting patient demographics are influencing health care delivery across the country. A diverse patient population with varying needs, values, lifestyles, socio-economic backgrounds and priorities is driving the need for more customized care solutions. Health care consumers are taking a more active role in their care experiences by using technologies such as online patient portals, telemedicine, electronic medical records and online bill pay and appointment scheduling, all of which are empowering patients to better manage their own health.
Even before the pandemic, new models of health care delivery were emerging, offering consumers convenience and accessibility to local care. An influx of non-traditional, retail-related companies have been entering the market, including Amazon, Walmart, and Apple in addition to existing retail clinics. As patient expectations and demographics change, hospital systems need to evolve the traditional model of care to compete with new players in the marketplace and cater to shifting consumer demands.
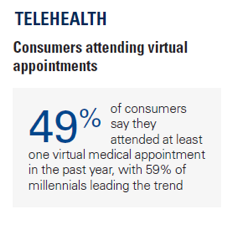 Convenience is one of the top trends driving the new post-Covid health care environment. For example, over the past several years telehealth use exploded, with 49% of consumers stating that they have attended at least one virtual medical appointment in the past year. Of note, millennials are the biggest users of telehealth at 59%, according to Environmental Scan 2023. Patients continue to demonstrate that access to quality care close to home, either virtually or in person, with reduced waiting time for appointments, is important.
Convenience is one of the top trends driving the new post-Covid health care environment. For example, over the past several years telehealth use exploded, with 49% of consumers stating that they have attended at least one virtual medical appointment in the past year. Of note, millennials are the biggest users of telehealth at 59%, according to Environmental Scan 2023. Patients continue to demonstrate that access to quality care close to home, either virtually or in person, with reduced waiting time for appointments, is important.
To keep up with the shift in consumer trends, including the rise in new competitors, digital tools and even social media, health care leaders need to collect, analyze and use valuable patient experience data to determine how to best personalize care delivery. Adopting Artificial Intelligence (AI) tools in areas such as clinical care and business operations is a must to accurately and efficiently manage the plethora of data as it continues to grow. Patient experience data is especially useful for marketing health care services in a way that speaks directly to the unique needs of different age groups and communities to attract the diverse patient population to hospital systems.
Creating a culture of trust
In addition to the patient experience, creating a culture of trust and building relationships between patients and providers, as well as between clinicians and the organizations that employ them is important for success. Health care is very personal: Patients who trust and develop long-term relationships with care providers typically have better overall outcomes, and in tandem, hospitals see higher patient satisfaction and loyalty among both patients and staff.
Health equity
Health equity in underserved and marginalized communities has been a top concern for health care systems for many years. The pandemic shined a new spotlight on the issues of diversity, equity and inclusion. Playing a major role in the well-being of diverse populations are social determinants of health. Lack of access to affordable health care, unemployment, food insecurity, racism and other socioeconomic and societal inequities have negatively impacted communities of color and lower income populations.
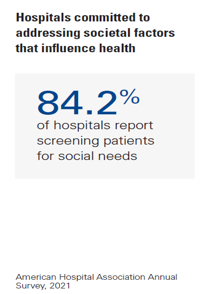 Hospitals and health systems have been active in addressing inequities and reducing disparities through robust community outreach programs and partnerships to impact the well-being of the underserved. Hospital leaders remain committed to addressing societal factors that influence health, with 72% of hospitals reporting having at least one program or strategy to address social determinants of health in their communities and more than 84% of hospitals screening patients for social needs, according to Environmental Scan 2023.
Hospitals and health systems have been active in addressing inequities and reducing disparities through robust community outreach programs and partnerships to impact the well-being of the underserved. Hospital leaders remain committed to addressing societal factors that influence health, with 72% of hospitals reporting having at least one program or strategy to address social determinants of health in their communities and more than 84% of hospitals screening patients for social needs, according to Environmental Scan 2023.
This engagement will need to be expanded over the coming years to address health inequities and to increase opportunities for inclusion and access to care throughout the communities served.
Planning Now for the Next Public Health Crisis
At the peak of the pandemic, hospital surge capacity plans were stressed to an extreme, posing many operational and financial challenges. One of the greatest lessons learned from the pandemic is preparedness. Looking forward, hospital executives must work to stay ahead of the next public health crisis, continuing to develop plans for surges in demand in addition to ensuring access to medical supplies and adequate staffing during periods of extreme need.
Preparation must also include more robust plans for cyberattacks. According to John Riggi, national advisor for cybersecurity and risk for the American Hospital Association, "cyberattacks represent the greatest external threat to clinical operations.” Ransomware attacks, phishing attempts, and data breaches reveal the vulnerability of hospital systems and the calamity that can follow such attacks, he adds. By implementing security protections, layered technical defenses, and having systems in place to swiftly respond to cyber threats hospital leaders can stay ahead of future risks.


