DIGITAL STRATEGY
How to Seamlessly Deploy Digital Solutions in a Post-Covid Future
Taking a broad organizational approach that aligns digital deployment strategies with larger organizational strategies will position hospitals and health systems for future success.
Using digital technology should feel seamless by now. With the accelerated online way of living brought on by the COVID-19 pandemic, people are using digital tech more than ever to accomplish everyday tasks — like working from home, ordering takeout and grocery shopping. It is no surprise that the same ease of use is expected of digital health technology. However, in this space, the transformation has been an uneven process.
While health care providers across the nation rapidly scaled their virtual care services during the peak of the pandemic, deploying digital technology has had its challenges.
“Transformation has been elusive,” said Karen Murphy, PhD, RN, executive vice president & chief innovation officer and founding director of the Steele Institute for Health Innovation at Pennsylvania-based Geisinger, when describing the deployment of digital solutions during a recent episode of AHA Transformation Talks. “In the past, we looked at digital technology first and not the problem we were trying to solve. At Geisinger, we are looking at the problem first and the technology second.”
Before the COVID crisis, hospital and health systems were also taking a project-by-project approach to their digital strategies.
“Hospitals often look to digital technology to solve specific, but sometimes narrow problems,” said Lindsey Dunn Burgstahler, vice president at American Hospital Association (AHA) Center for Health Innovation. “While it’s critical that technology investments solve specific problems, it’s also crucial that they come together in a seamless and holistic user experience. Otherwise the result can be a fragmented experience.”
Although patients are more open to using digital technology as part of their care, health care providers and physicians continue to face obstacles.
“Switching between multiple programs to chart patients can be cumbersome,” said Sandeep Wadhwa, MD, MBA, global chief medical officer of 3M Health Information Systems Inc. “We need to simplify the digital experience to the point of care.”
In addition to the burden of unsynchronized tools, studies show using digital health solutions can alter clinician workflows and contribute to burnout while taking time away from provider-patient interaction.
Still, clinicians see value in digital tech solutions.
“The digitization of health care, which began with the implementation of EMRs, benefits patients and clinicians by improving the accessibility of health data — and the insights that can be derived from that data,” said Dunn Burgstahler. “While many clinicians are frustrated with the administrative burden of EMRs, more and more technologies are becoming available to help reduce that burden.”
According to a 2020 survey from the Deloitte Center for Health Solutions, primary care physicians and specialists said they would find the following advanced technologies “extremely valuable”:
- 48% see advantages in deploying smart devices in exam rooms that automatically record blood pressure, ultrasound and other readings into the electronic health record (EHR).
- 48% believe that using digital technology is beneficial in ambient voice-to-text translation for recording visit notes.
- 25% think that digital technology can assist in clinical decision-support to analyze patient symptoms, vitals and problems to suggest diagnosis possibilities.
While these technologies are new and not widely used across U.S. hospitals and health systems, they will continue to shape the future of digital health care delivery.
A 360 Degree View of Digital Deployment
To enhance health care outcomes, digital transformation must involve both patients and providers. Engaging key stakeholders, including senior-level executives and front-line caregivers who understand user perspectives and workflow impact, will align digital initiatives and investments.
“It is so important to look at all perspectives when deploying digital health care solutions,” said Dunn Burgstahler. “There is a need to make care more convenient and coordinated, but the backend workflow also has to be digitally transformed, so you need to look at the entire picture and all perspectives.”
She recommends hospitals and health systems identify a champion to oversee the complete digital process.
“What we have now are a lot of technologies that are solving problems, but they are somewhat narrow-use cases. If we keep deploying new technologies for narrow-use cases, they are going to create problems for clinicians. So there needs to be someone to understand the perspectives from all angles.”
A designated digital champion would also help align strategies with organizational strategic plans.
“Having a champion or clear leader with authority and responsibility for the digital experience can help reduce friction for patients and clinicians,” said Dunn Burgstahler. “In addition, a digital leader can help ensure that the evaluation and selection of digital tech investments aligns with the organization’s strategic plan. This increases the likelihood digital investments are solving the most pressing health needs for the community rather than a narrower problem that happens to have a vocal champion.”
Gaining a deeper understanding of clinician challenges with digital solutions is key for evaluating viable options.
Improving Outcomes with Digital Solutions
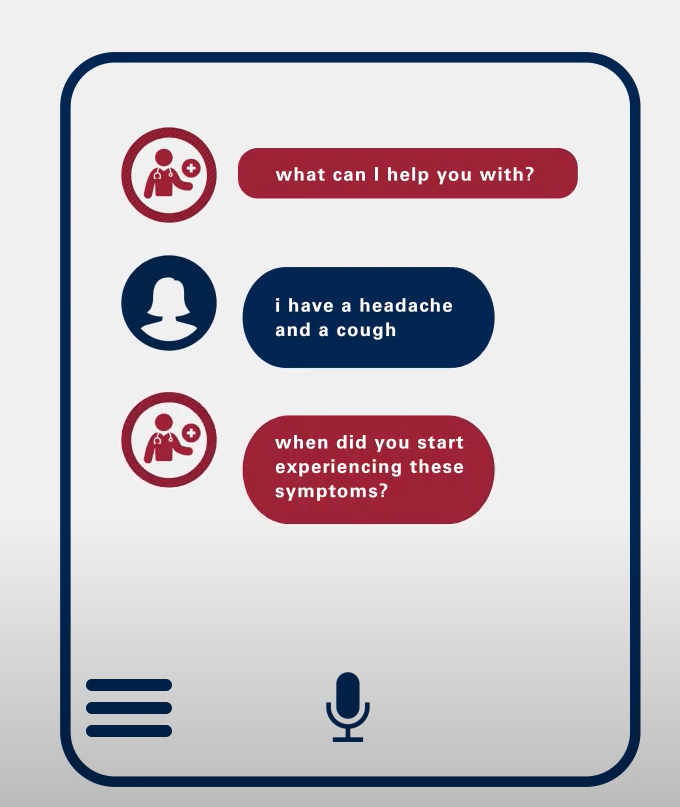
Powerful digital technologies and tools like robotic process automation, voice recognition and virtual care platforms, many of which are powered by artificial intelligence and machine learning, can be applied to increase efficiency, support clinical decision-making and improve outcomes. Increased use of smart-phones, wellness tracking and remote-monitoring devices are also giving clinicians a more consistent and complete picture of a patient’s health status.
For example, Geisinger used digital solutions to improve communication with patients during the pandemic.
“It’s important to adopt the thinking of the disrupter experience,” said Dr. Murphy. “The pandemic has accelerated digital adoption and demonstrated the value of digital technology in keeping in contact with patients.”
Another common digital technology valued by clinicians is ambient voice systems that translate and record documentation notes.
“Doctors are spending equal time seeing patients as time spent documenting their care,” said Dr. Wadhwa. “This contributes to physician burnout.”
Voice-to-text technology may also help foster better patient-provider communication, as research shows less computer note-taking drives stronger patient interactions. According to a 2005 study of the impact of exam room computers on clinician-patient communication, it was found that computer usage can create a barrier to effective relationship building and maintenance between clinician and patient. Ambient voice systems may remove that barrier.
Digital solutions, such as virtual care and remote patient monitoring, may also help lower the total cost of care and increase convenience.
“Patients with chronic conditions can be monitored remotely and benefit from convenience, while clinicians benefit from collecting more data on the patient’s condition,” said Dunn Burgstahler. “This is particularly helpful among patients who face challenges getting to regular appointments. Remote monitoring gives clinicians an opportunity to intervene earlier when health status changes, thereby heeding off a worse condition, which could lead to increased costs.”
When deploying digital solutions, the advantages of taking a broad organizational approach aligning to larger organizational strategies will prove beneficial to the future of health care.
Learning More
- This article features content from an AHA Transformation Talks video, “Deploying Digital Solutions to Enhance Care Delivery and Outcomes”
- AHA Transformation Talks, a series of video discussions among health care thought leaders, offer insights to help hospital and health systems navigate health care’s new, disruptive environment and prepare for what’s next.
- Each 10-minute video in this series focuses on a transformational topic explored by the 2021 AHA Environmental Scan and SHSMD's Futurescan 2021-2026: Health Care Trends and Implications.
This article features interviews with:
Lindsey Dunn Burgstahler
Vice President, Programming and Intelligence
AHA Center for Health Innovation
Chicago, Illinois
Karen Murphy, PhD, RN
Executive Vice President and Chief Innovation Officer, Founding Director
Steele Institute for Health Innovation
Danville, Pennsylvania
Sandeep Wadhwa, MD, MBA
Global Chief Medical Officer
3M Health Information Systems Inc.
Denver, Colorado