STRATEGIC PLANNING
Consumer Responsiveness: Principles to Transform Health Care Experiences
It is known that Americans frequently compare prices for purchases, but most people with insurance tend to overlook cost when it comes to health decisions. Instead, most place greater emphasis on the expertise of health care providers and organizations and the overall experience that they offer.
In a presentation during the SHSMD Connections Conference 2023 in Chicago, last September, David Grady, the national vice president—innovation, at Kaiser Permanente, and Dan Miers, the chief strategy officer at Unlock Health, discussed the shift from “health care consumerism” to “consumer responsiveness health care”—the latter of which emphasizes empathy, clear communication and an understanding of patients’ health behaviors and needs.
A Shift Away From Health Care Consumerism
When Miers presented at the SHSMD Connections annual conference in 2016, the conversation focused on health care consumerism—the idea that Americans approach health care options similarly to how they approach other purchases.
However, as most quickly realized, “health care is not a commodity,” Miers notes.
In a market that is truly consumer-driven, five factors must be present:
- varied options;
- awareness of choice;
- transparency of information for choice comparison;
- a personal interest in the financial aspect of the purchasing process; and
- an ability to make a confident, calm and nonurgent choice.
Not all these factors are present in health care, Miers explains. For example, “we’re really good at options: There are lots of hospitals, lots of health systems, lots of care options. … But a key component that is present when someone is shopping for a product or a service is awareness that you have a choice. … If you're sitting in your doctor’s office and he says that you might have leukemia, you’re not sitting there going, ‘What are my choices?’ [The care process makes] the decision for you.”
Unlock Health’s mission is to help health care organizations create meaningful connections between consumers and care, with the ultimate goal of helping people improve their lives. “And that requires health care providers to deliver what people need and what they want,” says Brandon Edwards, the CEO and founder of Unlock Health.
A Shift to Consumer Responsiveness Health Care
The concept of “consumer responsive health care” highlights the importance of understanding patients’ health care journey, instead of treating health care as a series of transactional decisions (Figure). It is guided by five principles, according to Miers:
- “Know me, help me”: Anticipate patients’ needs and show compassion.
- “Make it simple for me”: Improve access and guide patients along the health care journey.
- “Treat me fairly”: Protect patient data and be transparent.
- “Show that you value my business”: Resolve patients’ needs and personalize experiences.
- “Inspire me to share”: Delight patients so they share their experience with others.
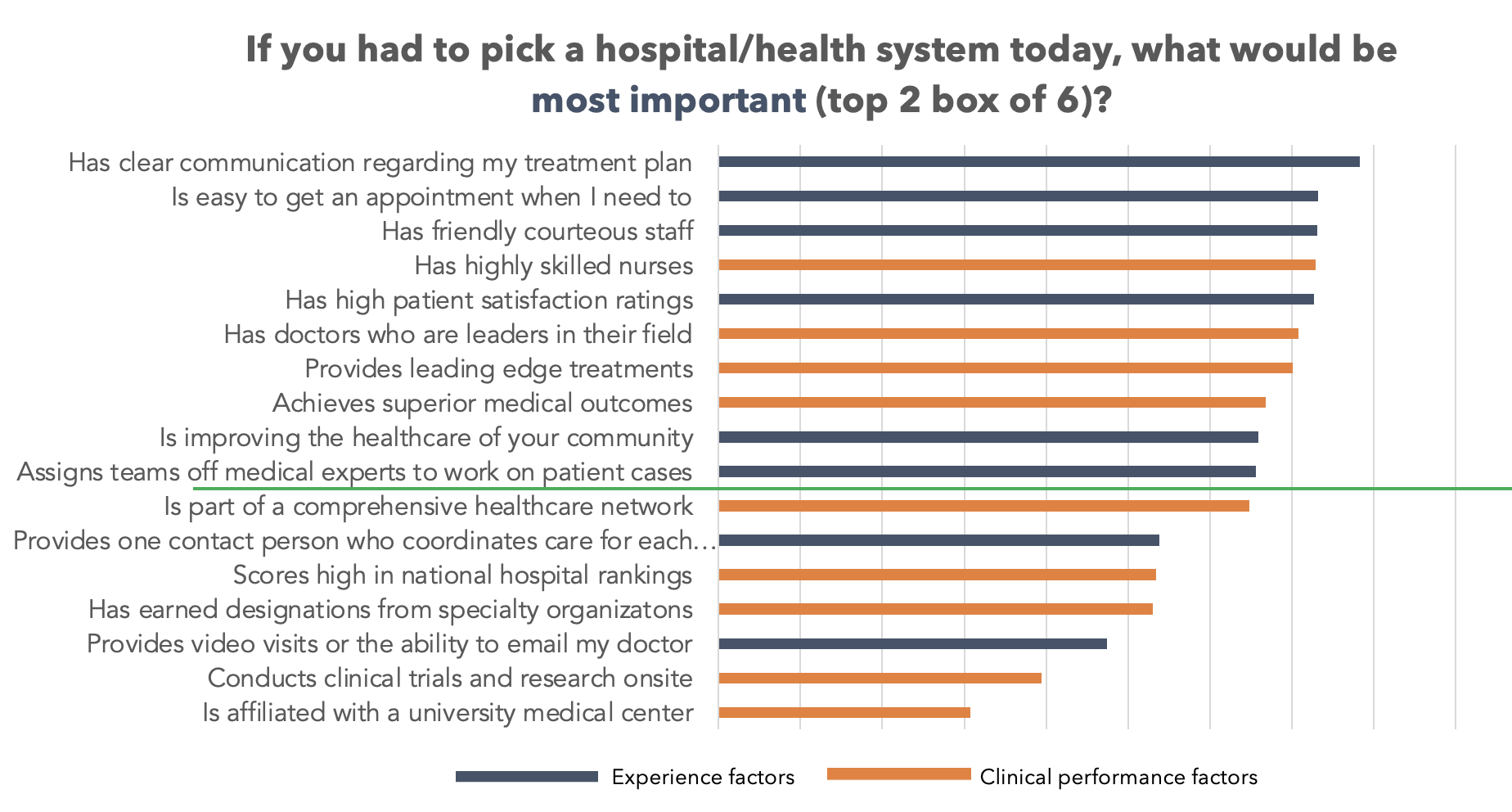
Regarding the last principle, Miers notes that reviews of health care organizations are happening whether or not these systems allow such feedback on their websites. Word of mouth is still the No. 1 factor driving patient selection, which is strange in an industry awash in data and objective standards of quality. Sadly, they are neither well understood nor embraced by consumers or the groups that provide them information (payors, hospitals and trade groups).
“We work with a number of clients where we go to online message communities and look at what people are saying about the brands,” he says. “How do we exceed patients’ expectations and inspire them to tell good stories about you? How do we host those stories and curate those stories ourselves on our platforms?”
Adopting Consumer Responsiveness Health Care Within an Organization
Kaiser Permanente has embraced the guiding principles of consumer responsive health care for more than a decade.
“This has been a journey for our organization for a number of years,” Grady notes. “A KP member doesn’t care how we organize or whether their needs require multiple functional silos—or what we refer to as ‘cylinders of excellence’—to work together or not. They care about experience, how their journey is managed, how quickly their problem is resolved. How do we either break down or connect across cylinders of excellence within the organization? [The guiding principles of consumer responsive health care are] essentially designed to do just that.”
Emphasizing Patient Experience and Clinical Indicators
Organizations that prioritize consumer-centric solutions can differentiate themselves from competitors, improve patient engagement and satisfaction, build trust-based and enduring relationships with their patients, and ultimately foster better health outcomes and more sustainable operations.
Kaiser Permanente has used digital tools, including partnering with organizations like Calm, to provide digital care experiences for patients with mental disorders such as anxiety and depression. Approximately 44,000 Kaiser Permanente patients were referred to digital apps and tools for additional mental health care experiences by their health care providers.
This integrated, consumer-centric approach resulted in 62% of Kaiser Permanente patients staying engaged with the app after three months, which is significantly higher than the national user retention rate for mental health apps. However, it’s crucial to balance consumer-centric solutions with the well-being of clinicians, as increased digital interactions can lead to burnout.
“It’s no good for our organization when our clinicians are leaving the profession,” Grady says. “We need to balance a member’s desire to interact with physicians digitally and be clear about the implications [of any consumer-centric solution] to operations and to our clinical workforce.”
Kaiser Permanente also aims to continue “phygital” experiences—a seamless combination of three domains:
- the digital platforms and channels in which consumers engage for care and other needs (e.g., scheduling, billing);
- consumers’ direct, in-person care experiences with clinical providers; and
- the physical spaces where consumer engagement occurs (e.g., hospital, clinic, community).
“As part of our app, we have a connection between the online and in-person pharmacy [in which] members can refill prescriptions. ... [A member] can get a text message ahead of time that says, ‘We’ve received your order. And your order is ready for pickup.’ [That’s] full transparency,” Grady explains. “When that member arrives, there’s a pretty seamless process for them to retrieve those [medications]. … We also have mail-order options where certain medications can be delivered to the home. During the pandemic, many cardiac rehab patients didn’t want to come into the hospital. Through a digital remote patient monitoring solution, members participate in rehab and a human monitors the data and does follow-up if someone isn’t following the program or there is a problematic variance; … everything is monitored remotely.”
Kaiser Permanente also employs a journey-based health care approach to enhance the entire experience of its members, from selecting Kaiser Permanente as the provider to clinical interactions and understanding benefits.
Furthermore, Kaiser Permanente realized that funding outcomes rather than projects was crucial. Traditional project-based funding often leads to lengthy initiatives that don’t adapt to changes, resulting in minimal impact. By shifting to outcomes-based funding, Kaiser Permanente can be more agile, test different approaches and focus on achieving measurable business impact.
By embracing the principles of consumer responsive health care—that is, anticipating patients’ needs, simplifying access, protecting patient data, personalizing experiences and exceeding expectations—Kaiser Permanente continues to improve its end-to-end journey for members while also delivering high-quality outcomes.